The heart, a tireless workhorse, tirelessly pumps blood throughout the body, ensuring the delivery of oxygen and nutrients to every organ. However, like any intricate mechanism, the heart can malfunction, leading to various conditions, including left ventricular failure (LVF) and right ventricular failure (RVF). These two conditions, while sharing the common thread of heart failure, exhibit distinct characteristics and consequences. Delving into the intricacies of LVF and RVF empowers individuals and healthcare providers to recognize their signs, understand their implications, and pursue appropriate treatment strategies.
Left Ventricular Failure: The Struggle to Pump Blood
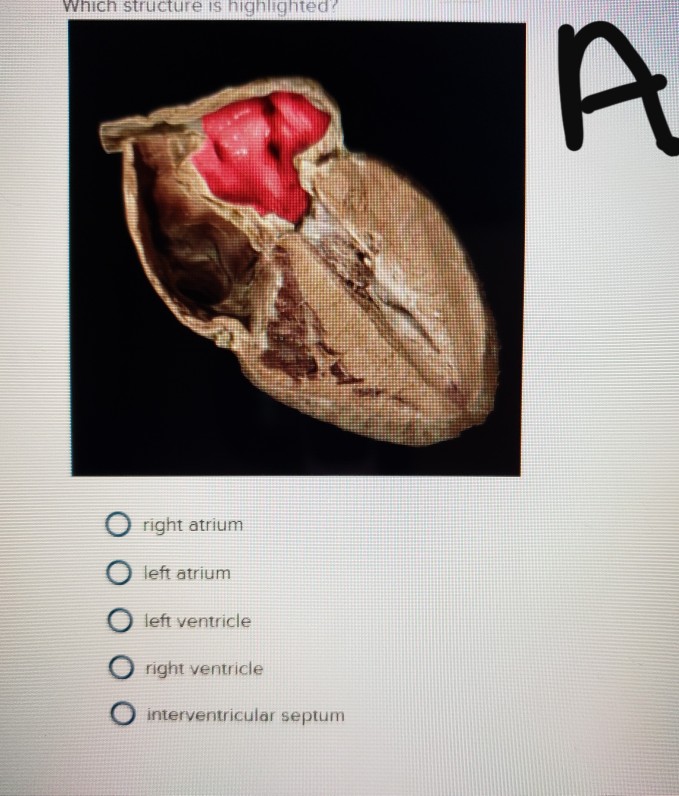
The left ventricle, the heart’s main pumping chamber, plays a crucial role in propelling blood into the systemic circulation. LVF arises when the left ventricle weakens or stiffens, impairing its ability to effectively eject blood. This reduced pumping capacity results in a buildup of blood in the left ventricle, leading to a cascade of adverse effects.

Symptoms of LVF:
- Shortness of breath, especially during exertion
- Fatigue
- Swelling in the legs, ankles, and feet
- Persistent cough
- Irregular heartbeat
- Chest pain
Consequences of LVF:
- Increased risk of heart attack
- Stroke
- Sudden cardiac death
Right Ventricular Failure: A Burden on the Right Side
The right ventricle, the heart’s secondary pumping chamber, performs the critical task of sending blood to the lungs for oxygenation. RVF occurs when the right ventricle weakens or loses its ability to effectively pump blood, leading to a buildup of blood in the right side of the heart and the lungs.
Symptoms of RVF:
- Swelling in the legs, ankles, and abdomen
- Swollen liver (hepatic engorgement)
- Jugular vein distension (prominent neck veins)
- Shortness of breath
- Fatigue
- Chest pain
Consequences of RVF:
- Pulmonary hypertension (high blood pressure in the lungs)
- Liver damage
- Right-sided heart enlargement
- Increased risk of pulmonary embolism (blood clot in the lungs)
Distinguishing LVF from RVF: A Diagnostic Challenge
The diagnosis of LVF and RVF often relies on a combination of clinical assessment, imaging techniques, and blood tests. While some symptoms, such as shortness of breath and fatigue, can be common to both conditions, other signs may provide clues to the underlying dysfunction. For instance, jugular vein distension and hepatic engorgement are more prevalent in RVF, while chest pain and irregular heartbeat are more closely associated with LVF.
Imaging modalities, such as echocardiography and electrocardiography (ECG), play a pivotal role in confirming the diagnosis and assessing the severity of LVF and RVF. These techniques provide detailed images of the heart’s structure and function, enabling healthcare providers to evaluate the pumping capacity of the ventricles and identify any abnormalities.
Treatment Strategies: Addressing the Underlying Causes
The treatment of LVF and RVF focuses on managing the underlying causes and alleviating symptoms. Lifestyle modifications, such as dietary changes, regular exercise, and smoking cessation, can significantly improve heart health and reduce the burden on the heart. Additionally, medications, including diuretics, beta-blockers, and angiotensin-converting enzyme (ACE) inhibitors, may be prescribed to manage fluid buildup, reduce blood pressure, and improve heart function.
In severe cases of LVF or RVF, more aggressive treatment options may be considered. These include surgical interventions, such as valve repair or replacement, and mechanical circulatory support devices, such as ventricular assist devices (VADs), which help the heart pump blood more effectively.
Conclusion: Understanding the Spectrum of Heart Failure
LVF and RVF represent two distinct manifestations of heart failure, each with its unique set of symptoms, consequences, and treatment approaches. Recognizing the early signs of these conditions is crucial for prompt diagnosis and intervention, allowing for the implementation of effective treatment strategies to improve heart function, enhance quality of life, and reduce the risk of complications.